My Presentation at the IHDD Symposium
The culmination of my work at my Neonatal Neuroscience Lab internship this past summer.
As I mentioned last entry, this summer I have been doing an internship at the Neonatal Neuroscience Lab at the University of Washington. Yesterday, I presented my research at the Institute for Human Development and Disability High School Research Symposium at the UW and I wanted to walk you guys through my completed presentation.
Alzheimer’s disease is a chronic disease characterized by neurodegeneration and the buildup of amyloid proteins. It is also the 7th leading cause of death in the United States. Right now, 10% of people over 65 and it is estimated that over 42% of people over the age of 55 will develop dementia at some point. This means that Alzheimer’s disease is on its way to become a larger issue, so it is important to investigate ways to prevent Alzheimer’s disease.
Today I am going to be explaining how vitamin D supplementation could help prevent the onset of Alzheimer’s disease in people who are vitamin D deficient.
Vitamin D is a fat-soluble vitamin that is usually obtained naturally in the human body through exposure to the sun and is found in a few foods such as fish and eggs. Over 35% of the United States population is vitamin D deficient, making it a widespread issue. According to the NIH, vitamin D improves calcium absorbance in the body, making it commonly associated with bone health, but there are vitamin D receptors in the brain.
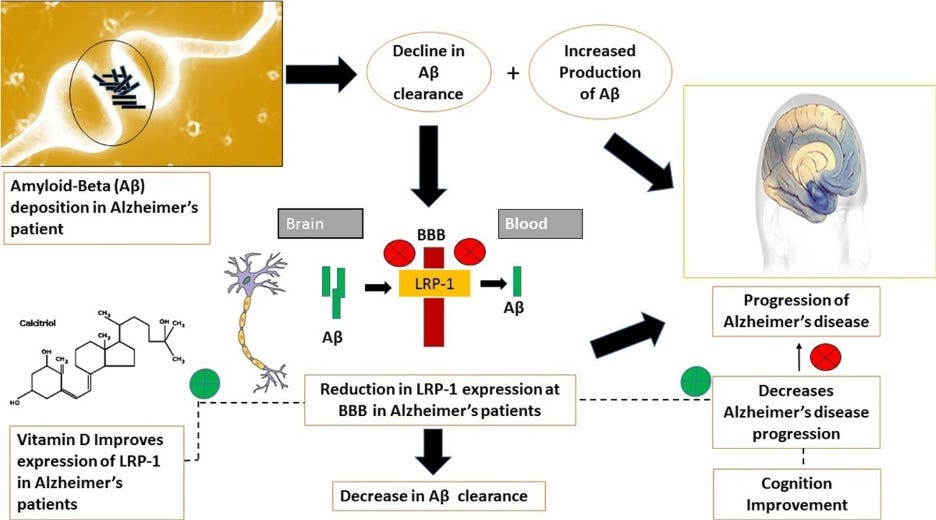
In the brain, vitamin D improves the expression of LRP-1. This is important because LRP-1 facilitates the movement of Amyloid-Beta proteins out of the brain. When LRP-1 expression is reduced (which could happen in a vitamin D deficient person), the Amyloid-Beta proteins can buildup in the brain. This is one of the things that leads to Alzheimer’s onset. Thus, vitamin D supplementation in deficient people could decrease buildup of Amyloid Beta proteins, decreasing rates of Alzheimer’s development.
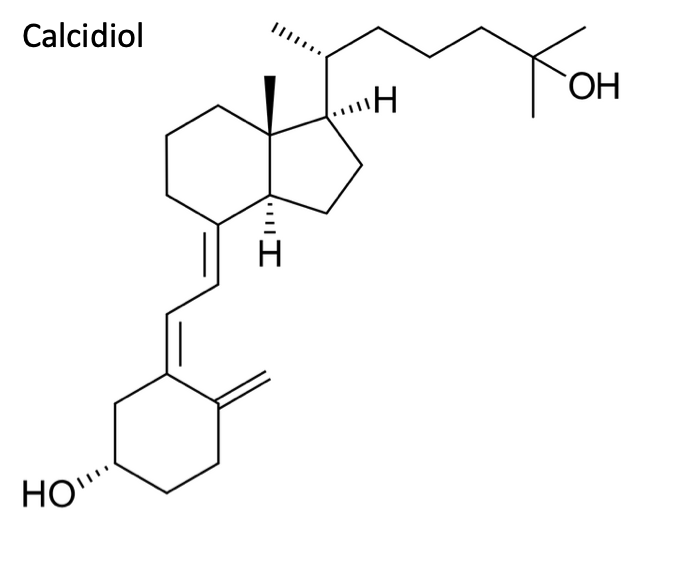
Above is calcitriol which is the form of vitamin D active in the previous diagram and is a steroid hormone and it’s the active form of vitamin D in the body. It finds to the vitamin D receptor that is found in the cell nucleus, and it is produced in the kidneys through the hydroxylation of calcidiol.
Calcidiol (one of the names for the storage form of vitamin D) is produced in the liver through the hydroxylation of vitamin D3, and this is what you measure to determine vitamin D deficiency.
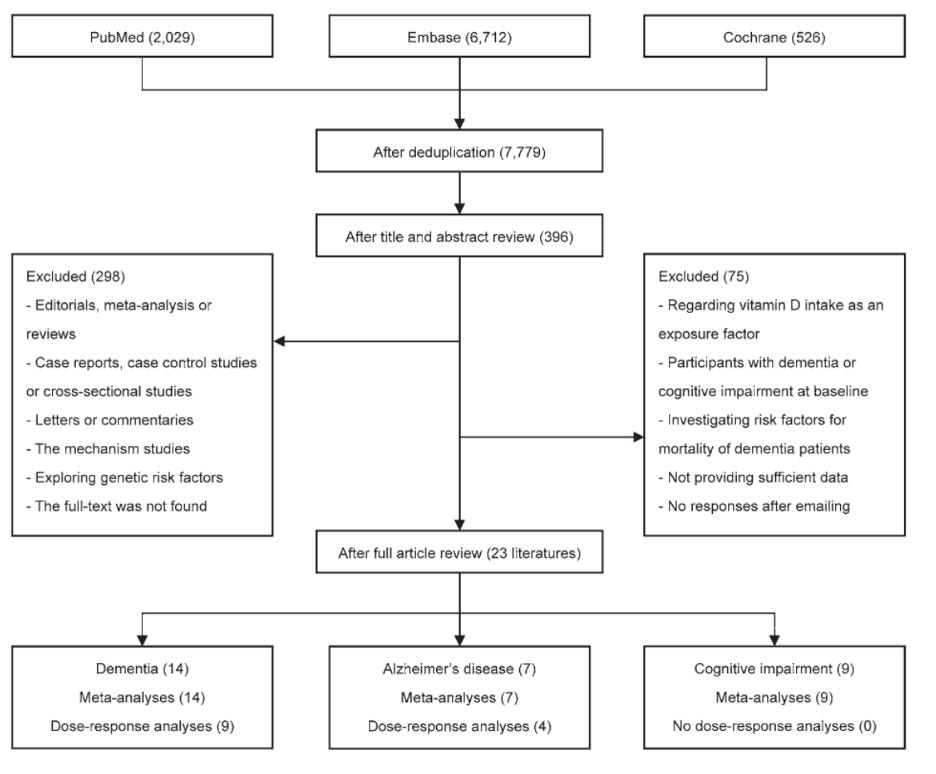
The first study that I looked at is a meta-analysis of many different studies that shows that vitamin D deficiency is associated with increased risk of Alzheimer’s.
The researchers eliminated studies from their pool based on baseline dementia, the threshold for vitamin D deficiency (the paper considers less than 75 ng/mL to be deficient), and a lack of sufficient data. 23 papers were ultimately identified, and the researchers ran Random Effect models to determine the level at which vitamin D deficiency is linked to the onset of dementia, Alzheimer’s, and cognitive impairment.
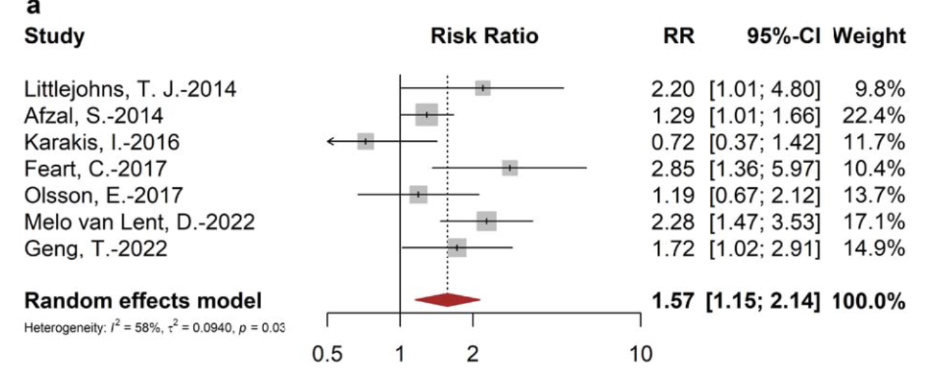
I focused on the result of vitamin D deficiency on Alzheimer’s patients. On the left are the different studies and on the right are the risk ratios and confidence intervals of said ratios. The random effects model found a risk ratio of 1.57. This means that, overall, people with vitamin D deficiency are about 50% more likely to develop Alzheimer’s than someone who is not deficient.
Since the meta-analysis demonstrates a correlation between vitamin D deficiency and Alzheimer’s onset, I found this animal study which demonstrates the helpful effects of vitamin D supplementation in providing neuroprotection against Alzheimer’s.
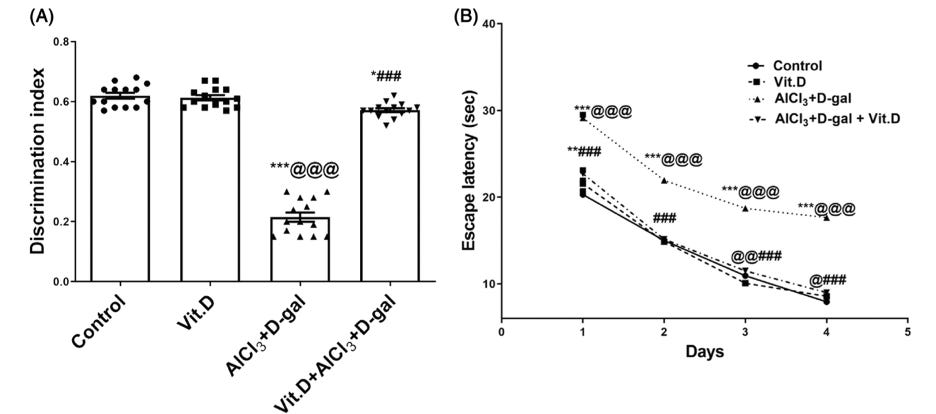
The researchers created an induced Alzheimer’s model in rats by feeding them aluminum-chloride-D-galactose (AlCl3-D-gal) which induced mitochondrial dysfunction. These mimicked effects of Alzheimer’s because mitochondrial dysfunction is a symptom associated with Alzheimer’s disease. The rats were split into four groups based on diet (a control, a vitamin D rich diet, the Alzheimer’s model diet, and a group fed both the vitamin D rich diet and the Alzheimer’s modeling one) and fed for 51 days. Then ten days were spent on behavioral trials.
The first graph is from a Novel Object Recognition test. The control, vitamin D groups along with the group that was fed both Alzheimer’s and vitamin D diets show much higher recognition of the old object compared to the rat group only fed the Alzheimer’s diet. This indicates that the vitamin D is providing neuroprotection against Alzheimer’s since the group being fed both diets shows higher memory levels than the Alzheimer’s only model. The second graph shows the results from a Morris Water Maze and the rats only fed the Alzheimer’s take much longer to find the escape platform than every other group which, once again, indicates that the vitamin D is providing neuroprotection since the group being fed both diets was able to find the platform about as quickly as the control group was.
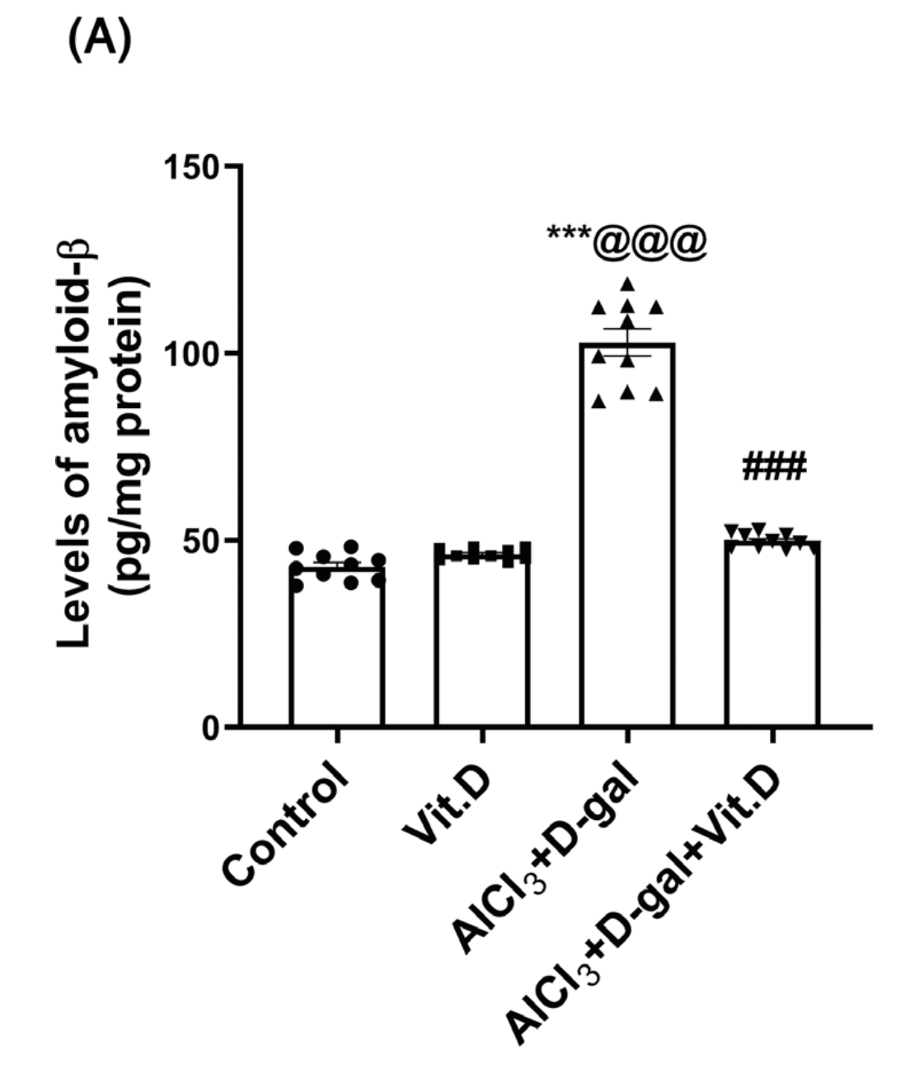
Then the researchers excised the rat brains to observe changes on the molecular level. The group only being fed the Alzheimer’s inducing diet shows higher levels of the amyloid beta proteins than every other group, indicating that the vitamin D is working to move the Amyloid beta proteins out of the brains in the rats fed vitamin D along with the Alzheimer’s inducing diet.
Once I found an animal model that supported the use of vitamin D in preventing Alzheimer’s, I wanted a study that looked into what happened in humans. What I found was the following study: Vitamin D Supplementation Worsens Alzheimer’s Progression: Animal Model and Human Cohort Studies.
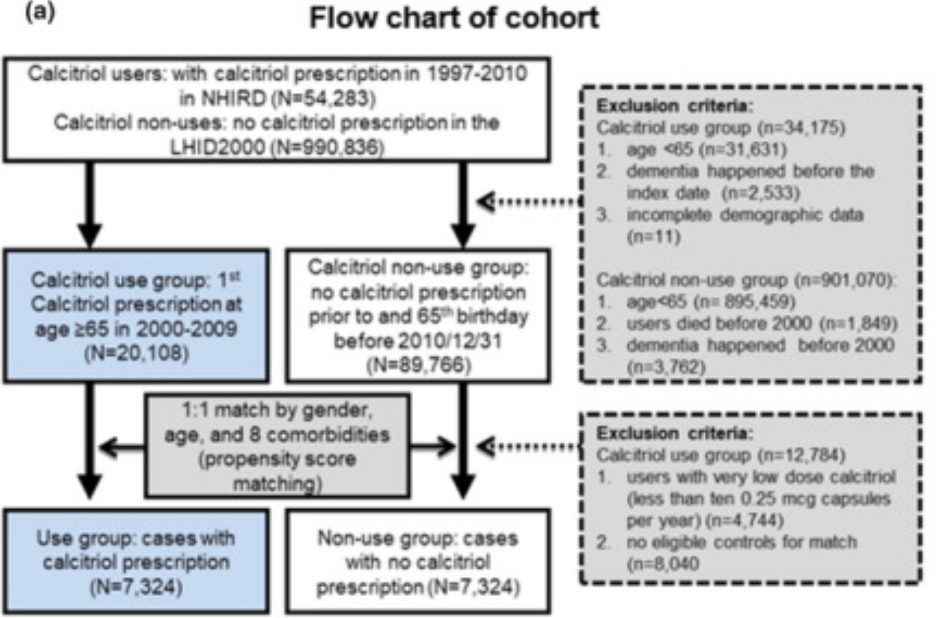
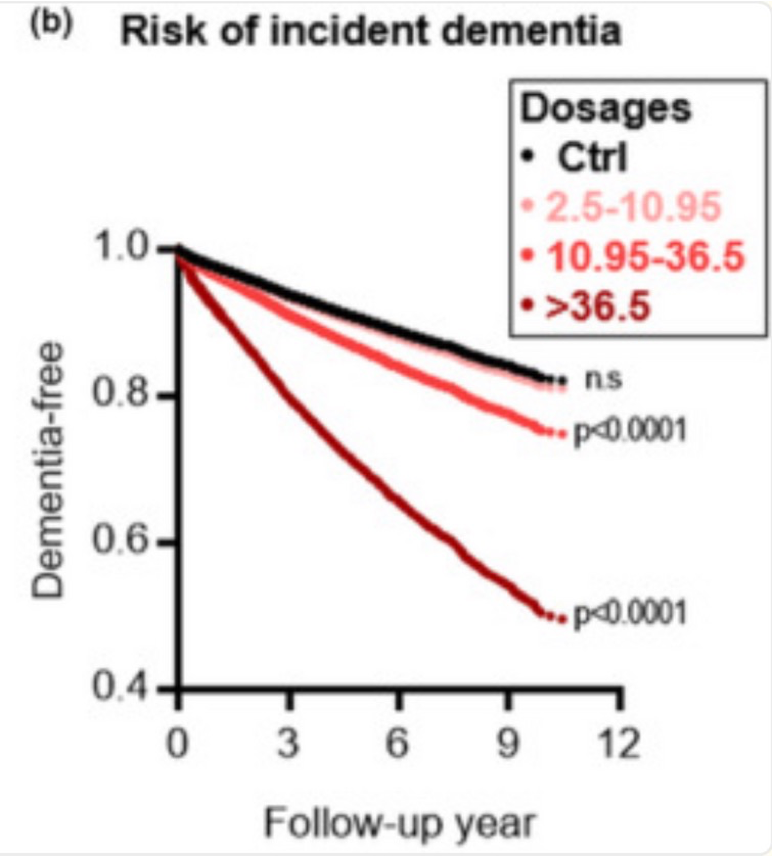
The researchers identified people from the National Health Insurance Research Database who were over 65 and dementia free before the year 2000 and assigned them to a treatment or control group. The treatment group had been prescribed calcitriol between 2000 and 2009, and the rate of dementia development was observed over 10 years.
This graph indicates that people taking over 10.95 micrograms instantly have increased rates of dementia. The thing is, this graph looks sketchy, since the change in dementia rates happens instantly. With something such as supplementation, the results are expected to take some time to show up. The instantaneous drop off indicates that the rates of dementia are caused by something other than the higher vitamin D dosage. For example, this study did not look at why these supplements were being prescribed, and people who are being prescribed vitamin D are the same people who are already at higher risk of Alzheimer’s due to poor health.
Because of that study’s questionable results, I found another human cohort study that did take into account backgrounds such as race, gender, and prior medical history when looking at the effects of vitamin D.
From the larger dataset, people were eliminated based on missing follow-up visits and already having dementia at the baseline. Then the study participants were split up into two groups, those taking no vitamin D supplements and those who were.
Here the blue line represents the people in the study exposed to vitamin D while the green line represents the people in the study not exposed to vitamin D. The group not exposed to vitamin D shows decreased dementia survival probability than the group exposed to vitamin D and this gap widens over time. The thing is, here this change is not instant, and the lines are aligned for about a year into the study. This provides kore confidence that the results are due to vitamin D supplementation rather than some external factor.
Overall, my studies show that vitamin D deficiency is associated with increased rates of Alzheimer’s and that vitamin D supplementation is associated with decreased rates of Alzheimer’s development. While my third study did have results indicating otherwise, this study also had issues.
Specifically, Study 3 did not account for the backgrounds of patients or why they were prescribed vitamin D. Since people prescribed vitamin D are already at higher risk of Alzheimer’s due to poor health, not accounting for that could have caused the differing results. Also, the other two papers looking at humans (study 1 and study 4) both consider prior health conditions and backgrounds when presenting their data.
In the future, researchers looking more into the role of vitamin D in Alzheimer's prevention could investigate whether the type of vitamin D (like calcitriol or calcidiol) impacts the extent of Alzheimer’s prevention. Additionally, one could look at whether the dosage of vitamin D impacts the level of neuroprotection provided. Study 3 did look at this, but since it had issues, it would be interesting to read a study that looked at dosage while still accounting for the patient’s backgrounds.
Thank you so much for reading!