Vitamin D and Alzheimer's
A look into my internship at the Neonatal Neuroscience lab at UW
This summer, along with my coding project, I am doing an internship at the Neonatal Neuroscience lab at the University of Washington. The goal of this internship is to learn the process of reading research papers to become informed of and draw your own conclusions about a topic. To do this we need to understand how to determine if a paper presents its data in a straightforward way and is not using statistical tests to make results seem more significant than they actually are (so essentially watching out for p-value hacking). Each student in the internship is assigned a mentor (an undergrad working at the lab) to go over papers with, ask questions, and get feedback. Throughout the summer, we have to present papers that we have found a minimum of three times. This creates a sense of community in the group and allows the two doctors in charge of the program to make sure that we actually understand what we are doing. At the end of the summer, we will present all of our findings as a review presentation to a panel of UW students and faculty.
The topic that I have chosen to study is the effect of Vitamin D supplementation on Alzheimer’s Disease. When we first introduced our topics, the doctor in charge of the internship gave everyone feedback about directions to go in. My feedback was that while my topic was interesting, I needed to make sure that what I was presenting wasn’t a “duh statement.” This is because Vitamin D is generally accepted to have positive effects on the brain, and me presenting on the beneficial effects of Vitamin D could seem unsubstantial. Last Thursday, I presented my first article. Keeping the feedback in mind, I specifically presented an article that showed that Vitamin D did not have a positive effect on Alzheimer’s Disease.
The article that I presented was called Vitamin D Supplementation Worsens Alzheimer's Progression: Animal Model and Human Cohort Studies by Lai et. al. To start off my presentation, I gave some background on Vitamin D and why it is important to look into possible Alzheimer’s treatments. Vitamin D is a fat-soluble vitamin obtained through sun exposure and foods such as fish and eggs. According to the NIH, vitamin D is associated with calcium absorbance in the gut and is important for bone health, and Vitamin D receptors are found in glial cells in the brain. This means that Vitamin D does have some impact on brain function. Alzheimer’s Disease is an increasing concern in the health of the elderly. Currently, 10% of people over the age of 65 and have Alzheimer’s, and according to an NIH article from February 2025, it is estimated that 42% of adults over 55 will develop dementia. On top of this, current medications used to treat Alzheimer’s target symptoms of the disease but do little to actually stop disease progression. Also, earlier observational studies have led people to believe that Vitamin D supplementation will provide neuroprotection against Alzheimer’s which is why it is important to do more tests to confirm this. Even more so since Vitamin D’s impact in the elderly is poorly understood.
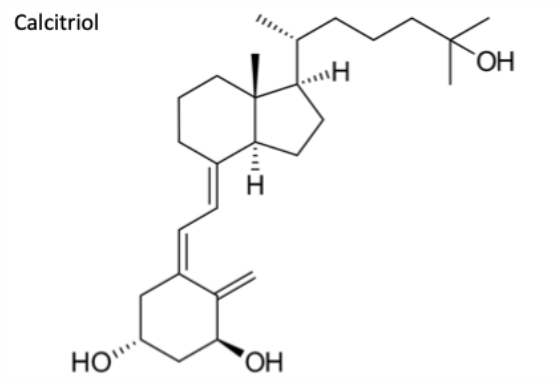
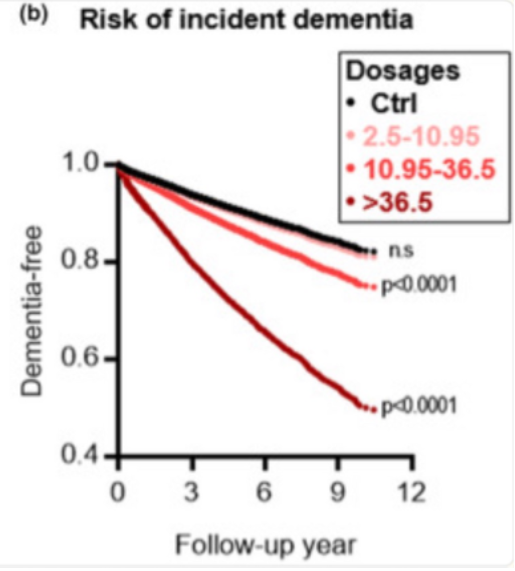
In the study that I presented, the researchers measured two forms of Vitamin D: Calcitriol and Calcidiol. Calcitriol is a steroid hormone and the active form of vitamin D. It is mde in the kidneys and binds to vitamin D receptor in cell nucleus. Calcidiol is the storage form of vitamin D and is produced in the liver via the hydroxylation of Vitamin D. This is what is measured to determine Vitamin D deficiency.
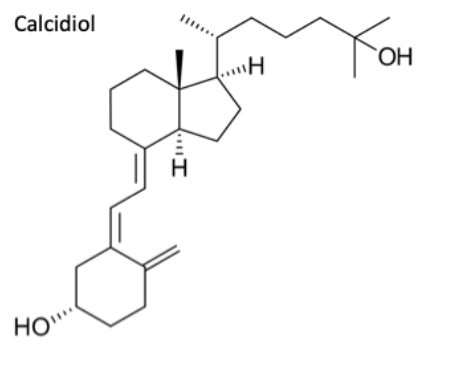
The first part of the study was an animal trial. The researchers used both wild type mice and a special type of mice called APP/PS1 mice. These mice were genetically modified to express a protein that is commonly associated in human Alzheimer’s patients to induce an Alzheimer’s like state on the mice. Both sets of mice were then fed a Vitamin D rich diet and observed in two-month intervals. The results showed that both four months and six months after the start of observation, the vitamin D levels in the APP/PS1 mice were significantly lower than that in the wild type mice. This could indicate that Alzheimer’s causes vitamin D deficiency. Additionally, cell cultures were taken from the APP/PS1 mice and exposed to Amyloid Beta proteins (a type of protein associated with the brains of Alzheimer’s patients) and either calcitriol or calcidiol. In both cases, there were significantly less viable cells as the dosage increased, indicating that calcitriol and/or calcidiol supplements may have a negative effect on Alzheimer’s patients.
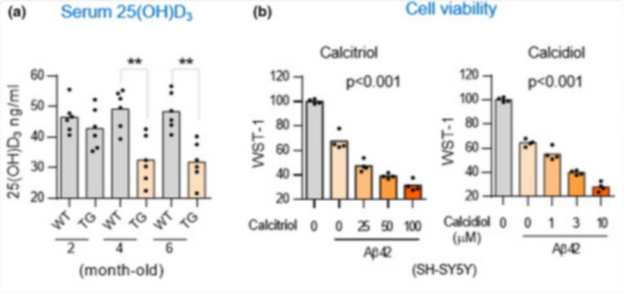
The next part of the study was two different human trials. The first used data from the National Health Insurance Database and the Longitudinal Health Insurance Database 2000 to observe the rates of developing Alzheimer’s for people over the age of 65 not prescribed calcitriol supplements compared to people who were prescribed calcitriol. The results indicated that people who did not take calcitriol supplements and the people prescribed the smallest doses of these supplements had relatively similar rates of developing dementia. Those who took supplements in doses of over 10.95 micrograms, however, were much more likely of developing dementia.
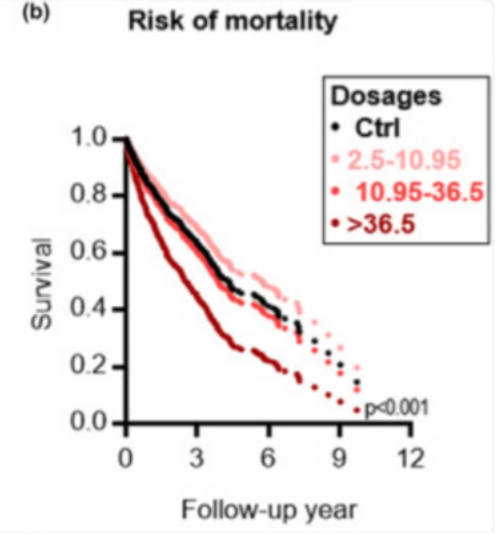
The third part of this study had a sample size of 980 people with dementia. 196 of them had a calcitriol prescription after developing dementia and the other 784 did not use calcitriol. The people were put in groups of one calcitriol user and four nonusers and groups accounted for age and gender. Interestingly, after being diagnosed with dementia, people that took the lowest dosage of calcitriol had a higher survival rate than people that took no supplements (as opposed to having the same rate of developing dementia). Still, those who took supplements of over 10.95 micrograms had a much lower survival rate.
After presenting the methods of the study, I went on to describe the possible limitations of it. Firstly, the study does not account for prior medical history, which means that it is impossible to factor in other causes for death. When I presented this to the group, the doctor in charge pointed out that people who are prescribed Vitamin D are usually getting such supplements because they have poor health already and are thus already at a higher risk for developing dementia. Also, the animal studies were done on mice which have very different brains from humans which means that the results from this study cannot necessarily be generalized to us.
Going forward, I want to research more about how Alzheimer’s progresses as a disease and how Vitamin D affects the brain in general. This way I will be more informed when I give my final presentation and be able to better understand the mechanisms behind the processes of Vitamin D impacting Alzheimer’s. And, of course, I need to read more articles about Alzheimer’s and Vitamin D to increase my understanding of the topic.


Excellent. A lot of these diseases like Alzheimer's are prion diseases. Meaning, proteins are misfolded. One of my earliest research projects was to study a protein called Apomyoglobin (without the Iron) and determine its structure as the chain length changes. So somewhere a pathway of the protein folding is being disrupted either during translation or post translationally when either the chemistry of the cell changes or some other regulator is off. Vitamin D is an interesting piece in the mix. Look for papers, where vitamin D in general affects protein structures and may be you can make a correlation.